Antibiotic resistance is a growing concern in the field of public health, with researchers warning of a potential catastrophic rise in infection-related deaths. A recent study conducted by Northern Arizona University, published in Communications Medicine, sheds light on the looming threat posed by multidrug-resistant bacteria.
According to lead author Benjamin Koch, the increase in antibiotic use worldwide has led to bacteria developing resistance to multiple antibiotics, known as multidrug-resistance. This poses a significant risk to the global population, as it increases the likelihood of death from infections. However, the real concern lies in the emergence of pan-resistant bacteria, which are resistant to all known antibiotics.
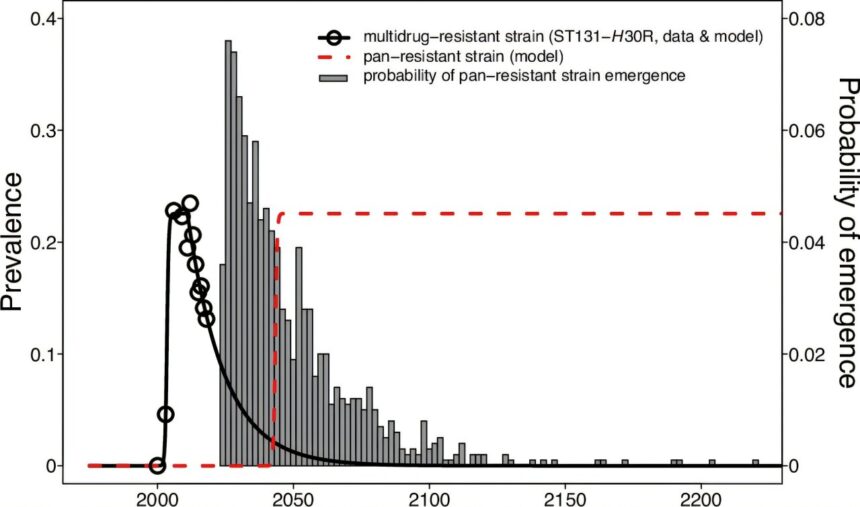
The research conducted by Koch and his team assesses the speed and magnitude of the expected impacts of pan-resistant bacteria. The results paint a grim picture of the future of public health, with a rapid and dramatic increase in infection-related deaths predicted once these bacteria become prevalent.
One of the key findings of the study is the potential impact of a hypothetical pan-resistant strain of E. coli on sepsis deaths in the United States. The models developed by the researchers show that sepsis deaths could increase by 18 to 46 times just five years after the introduction of such a strain. While this strain does not currently exist, the rapid evolution of bacteria means that it could emerge sooner than expected.
The implications of pan-resistant bacteria are far-reaching, affecting populations worldwide. This poses a significant challenge, as previously treatable infections could now prove fatal. Governments, industries, and individuals must take proactive measures to reduce the risk and slow down antibiotic resistance.
Governments can strengthen policies around the safe use of antibiotics in both food-animal and healthcare industries, as well as incentivize the development of new antibiotics. Technologies that monitor the emergence and spread of antibiotic resistance can also play a crucial role in combating this global threat.
On an individual level, it is important to use antibiotics only when necessary and as directed by a healthcare provider. Supporting policies that promote antibiotic stewardship and the development of new antibiotics is also essential. The authors of the study emphasize the need to reduce the factors that contribute to the evolution and dissemination of antibiotic-resistant pathogens.
In conclusion, the rise of antibiotic-resistant bacteria poses a significant public health threat that must be addressed urgently. By taking proactive measures at the governmental, industrial, and individual levels, we can mitigate the risks associated with antibiotic resistance and safeguard global health.