Male fertility is a topic of growing concern, with a recent study suggesting that medical conditions like sleep apnea may be contributing to a decline in male reproductive health. Published in Nature Reviews Urology, the study led by Dr. Tessa Lord from the University of Newcastle explores the impact of factors such as sleep apnea, varicocele, and high-altitude exposure on sperm quality and overall fertility in men.
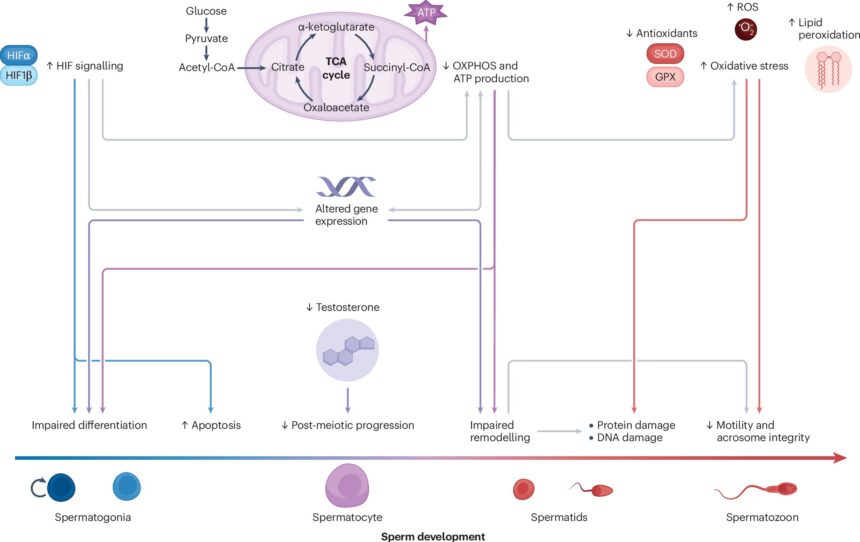
One of the key findings of the review is the role of testicular hypoxia in impairing spermatogenesis and sperm function. Testicular hypoxia, caused by conditions like varicocele and sleep apnea, reduces the level of oxygenated blood in the testes, leading to disruptions in hormone production and gene expression that can negatively affect sperm count and quality. Varicocele, a common abnormality in the scrotum, is a known cause of infertility in a significant percentage of men struggling to conceive.
Sleep apnea, a prevalent sleep-related breathing disorder, affects a substantial portion of the male population and has been linked to infertility in males. The review emphasizes the need for further research to understand the direct effects of sleep apnea on sperm production and quality. Additionally, high-altitude activities like hiking can also cause temporary testicular hypoxia, but the effects on fertility are reversible once oxygen levels are restored.
Dr. Lord highlights the importance of timely management of conditions like varicocele and sleep apnea to mitigate fertility risks associated with testicular hypoxia. Addressing underlying issues could potentially reverse subfertility caused by hypoxia and improve reproductive outcomes in men. Infertility and subfertility in men can have significant impacts on conception, underscoring the urgency of addressing these issues.
Furthermore, the study raises concerns about potential intergenerational effects of testicular hypoxia on male fertility trends. Evidence suggests that testis hypoxia in fathers could lead to developmental issues in embryos and fertility issues in their offspring. Despite advancements in understanding the relationship between hypoxia and fertility, there are still significant knowledge gaps that need to be addressed through further research.
Dr. Lord calls for continued efforts to uncover the broader implications of testicular hypoxia on male fertility and develop effective interventions to safeguard reproductive health for future generations. By improving fertility outcomes today and understanding the generational impact of testicular hypoxia, researchers aim to address the decline in male fertility observed over the past few decades.
In conclusion, the study sheds light on the complex factors influencing male fertility and underscores the importance of addressing testicular hypoxia as a critical issue in reproductive health. With ongoing research and awareness, there is hope for improving fertility outcomes and ensuring the reproductive health of men for generations to come.